A tight Achilles tendon, a condition marked by stiffness and limited flexibility in the band of tissue connecting the calf muscles to the heel bone, can be attributed to various factors. One prevalent cause is overuse or excessive strain, commonly observed in athletes who engage in repetitive activities, like running or jumping. Inadequate warm-up or wearing improper footwear during physical exertion can exacerbate tension in the Achilles tendon. Additionally, biomechanical issues, such as flat feet or abnormal foot arches, may contribute to tightness. Aging also plays a role, as tendons naturally lose elasticity over time, making them more susceptible to stiffness. Tightness can also result from injuries or inflammation, such as Achilles tendonitis. Ignoring the causes of a tight Achilles tendon may lead to discomfort and compromise overall foot health. If you have endured an Achilles tendon injury, it is strongly suggested that you visit a podiatrist as quickly as possible who can effectively treat this condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Comprehensive Foot & Ankle Center of South Jersey. Our doctors can provide the care you need to keep you pain-free and on your feet.
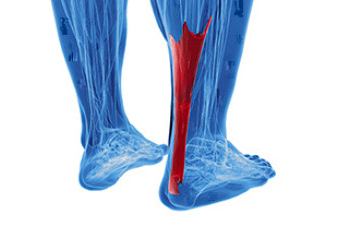
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Cherry Hill, Voorhees, Atco, and Turnersville, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.





